

Practice Administrator Cara Dennison began with Andover Family Medicine, in Andover, Kan.,18 years ago. Since that time, the practice has grown from a humble two-physician office to a thriving team of 14 clinicians.
In 2019, the organization made the strategic decision to join an Aledade accountable care organization (ACO). Today, the team participates in several value-based programs with Aledade, including the Medicare Shared Savings Program (MSSP) as well as contracts with Medicare Advantage and commercial plans, covering about 30 percent of the practice’s patient population.
Why did your practice decide to join Aledade?
We had been approached by another ACO that was forming in Wichita. That’s how we were first introduced to the concept. But Aledade seemed much more established and was a nationwide ACO. We felt it would offer us more opportunities and resources.
How was your transition to value-based care?
Change is always challenging. I’ve learned over the years, no matter what it is, people are used to doing things methodically throughout their day.
In the beginning, it was viewed as more work. Ultimately the staff and providers realized that these are all things we were already doing for our patients. We wanted to improve processes and measure outcomes.
We did change some workflows to make sure we were tracking things well and not missing anything. Now that’s our approach with every patient. Our philosophy has always been to treat every patient the same. It makes it easier for the staff if the same expectation is there. No matter who the payer or the patient is, they all need the same quality care.
How have you used the shared savings you’ve earned in the ACO?
We have added two care coordinators who focus on value-based care efforts, specifically transitional care management (TCM) and emergency department (ED) follow-ups. One is a medical assistant that’s been with us for close to 10 years and is very familiar with our patients. The other is a pharmacist who addresses all our medication adherence measures. She is also a great resource for medication reconciliation after hospital stays. The care coordinators do an excellent job, and that’s where we have made the biggest improvement in patient outcomes.
Both of our care coordinators give patients their direct phone numbers for after a hospital stay or ED visit. This is a huge advantage for the patients who require a little more of our time and attention. Whether it’s getting home health set up or questions about medication changes, often those things can be discussed on the phone before they come in for their visit with the provider.
What has the most impactful change you’ve made to your workflows?
We have created templates in our electronic health record (EHR) for when care coordinators make follow-up calls. The template is a reminder of all the questions they need to ask and things they need to look at in the records to provide all that information in one place for the provider before the follow-up appointment.
The templates have been helpful because a lot of times when you get a hospital discharge, there are 50 pages to go through, and it is difficult for the providers to go through it while the patient is here in the office. The care coordinators create a note, and then the clinicians can go through it with the patient.
How has being in an ACO changed your approach to patient care?
Preventive care has really moved to the top of our focus across the practice.
We are fine tuning our approach all the time. We have a gap list champion who knows the list inside and out. She messages the clinical staff to remind them which patients need preventive services like colonoscopies and mammograms.
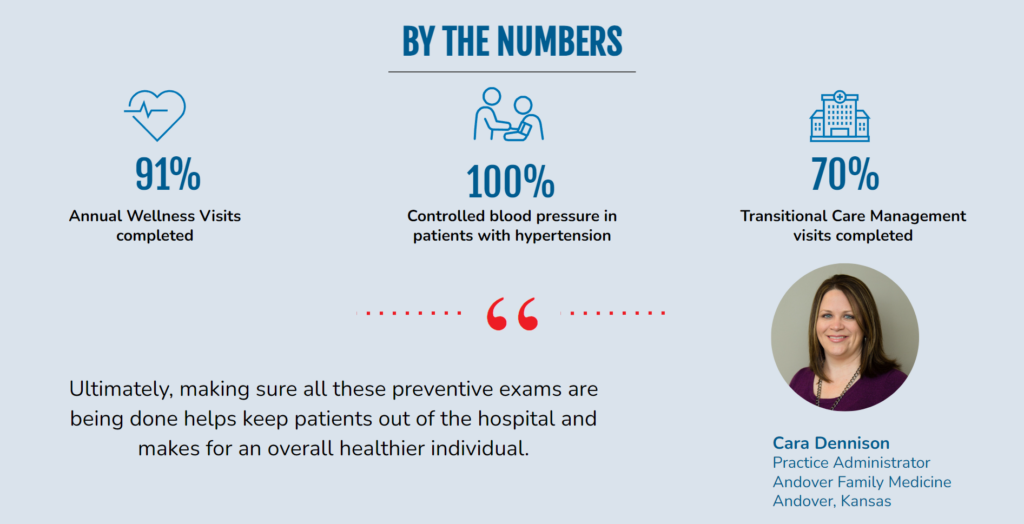
Ultimately, making sure all these preventive exams are being done helps keep patients out of the hospital and makes for an overall healthier individual.
