
Value-based care is the concept that health care clinicians should be paid for keeping people healthy rather than the volume of services delivered. The goal is to help patients maintain their highest possible level of wellness, rather than waiting until patients get sick to provide care, which is often more complex and expensive.
Aledade’s Co-Founder and CEO, Farzad Mostashari, has often likened value-based care to a waterfall. Today’s health care system is not designed to keep patients from “falling over the edge of the waterfall” with illness, but rather to respond rapidly and do whatever it takes to save those lives once they’ve gone over the cliff. Our system, he notes, will spare no expense to treat a stroke but, until value-based care, it spent nearly nothing to prevent that stroke in the first place.
That type of system leads to more than a trillion dollars in health care waste annually. While there may not be financial incentives at large to prevent individuals from falling over the edge, Travis Broome, Aledade’s Senior Vice President of Policy and Economics, has said that “the opportunity is enormous to stand at the edge of the waterfall. [Primary care has] the best aligned incentives to stand at the top of the waterfall and keep people healthier.”
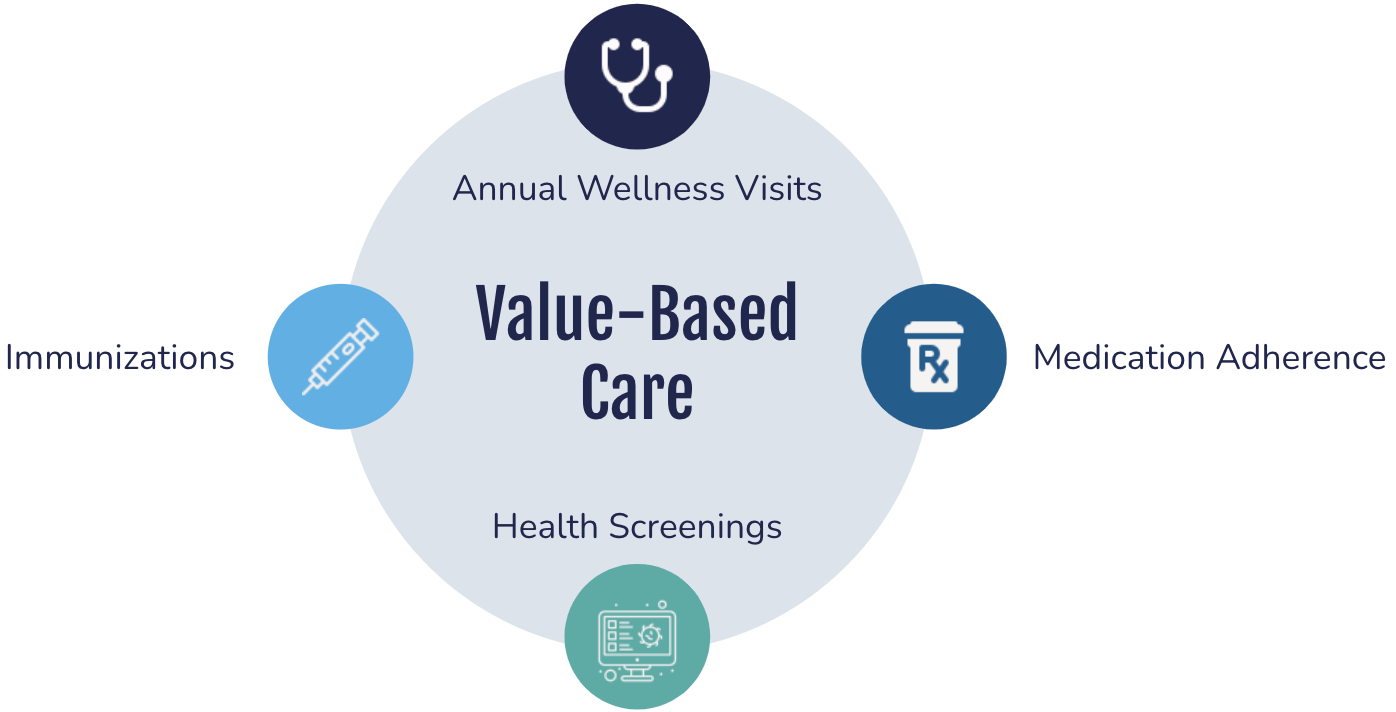 Providing patients with routine, preventive care and ensuring that their health care needs are met are vital to keeping patients healthy. Annual Wellness Visits present an opportunity to develop care plans, ensure that patients are adhering to their prescribed medications and up to date with their immunizations, and perform necessary health screenings.
Providing patients with routine, preventive care and ensuring that their health care needs are met are vital to keeping patients healthy. Annual Wellness Visits present an opportunity to develop care plans, ensure that patients are adhering to their prescribed medications and up to date with their immunizations, and perform necessary health screenings.
Accountable Care Organizations: An opportunity to reduce costs and improve health.
Accountable Care Organizations (ACOs) are made up of a group of primary care physicians, hospitals and/or other health care providers, who embrace accountability of the total costs and quality for an attributed population of patients.
Outside of value-based care payments, there are two major ways health care services are paid : fee-for-service, where only descriptive codes like those found in Current Procedural Terminology (CPT) handbook are eligible for payment; and grants. However, both have their respective limitations.
In ACOs, reimbursements are directly tied to quality metrics and reductions in the cost of care. Rather than following a set of strict requirements, ACOs create the opportunity for clinicians who are willing to step up and take accountability for their patients to be rewarded for innovation in generating improved outcomes.
Physician-led ACOs vs hospital-led ACOs: What are the differences?
Independent physicians in physician-led ACOs have a voice, have no conflict when it comes to keeping patients healthy and can quickly identify and solve problems. While financial alignment for hospital-led ACOs is good for value-based payment and the professionals working in these ACOs want their patients to stay healthy, it’s also counter to their bottomline — hospitals make a lot of money when someone falls over the waterfall.
Physician-led ACOs consistently and dramatically outperform hospital-led ACOs. In 2021, ACOs led by physician groups realized the most savings, at $224 per beneficiary, while also making up the largest cohort (45 percent). Hospital-led ACOs (27 percent) saw savings of $147 per beneficiary while the remaining ACOs, led by both physician groups and hospitals (28 percent), had savings of $156 per beneficiary.
Physician participation in accountable care continues to grow.
In early 2023, the Centers for Medicare & Medicaid Services (CMS) announced that over 13 million people with Medicare would be served by three innovative accountable care initiatives.
Brenda Vozza, MD, founder and physician at Brookridge Internal Medicine, and Aledade Local Medical Director, knew that participating in value-based care would be vital to her practice. With almost 25 years in private practice under her belt, she says, “I saw the writing on the wall years ago that this is what we needed to do to take care of patients. [Participating in value-based care] has really helped provide data so that I can actually do what I went to medical school to do: take good care of patients.”
Joining an ACO has helped enable Dr. Vozza to take the care she provides her patients “to the next level.” The data she receives enables her to have important conversations with her patients and engage in discussions about the care they are receiving outside of her practice and how she can help address some of their needs.
The shared savings her practice has earned as a result of adopting value-based care have also been put to good use: going towards improving technology, enabling a better patient experience, and unlocking new ways to recruit and retain top talent like bonuses for staff.
Section header: Bottom line: Value-based care is the right choice for patients and practices
Adopting value-based care can enable primary care organizations to improve patient care and lower health care costs, by keeping the patients they serve from falling over the edge of the waterfall.
Go more in-depth and learn more from Travis Broome and Dr. Vozza by clicking here.
Want answers to your value-based care questions? Schedule a custom consultation with our experts now.
