UPDATE: As part of our work to learn from our nationwide network of primary care professionals, and based on the latest in clinical expertise, we have since updated the Core 4. You can find the latest version here.
By Ahmed Haque
For a busy primary care practice or health center, the path to shared savings in value-based care can be difficult, especially for those trying to chart it on their own. Fortunately, as for seafaring captains, there are some fundamental tools – maps that can help make the journey away from fee-for-service health care an easier one.
Back in 2014, before launching Aledade, our co-founder and CEO Dr. Farzad Mostashari saw the need for these kinds of simple, straightforward best practices. “Lessons from successful physician-led ACOs,” he and his colleagues wrote, “must be widely and rapidly distributed.”
That’s why Aledade created the Core 4TM.
The Aledade Core 4 simplifies the complex goals of population health improvement. It distills the work of value-based care into four targeted initiatives that further population health and increase the chance that a practice will earn shared savings.
The Core 4 is built on a foundation of nearly a decade of experience from more than a thousand practices across the country in value-based contracts. Through the years, we’ve found that practices that excel in these four competencies tend to improve health outcomes for their patients and achieve savings.
But the health care landscape is always changing. Two of Aledade’s core values are evidence and curiosity. So, as the evidence changes and as we ask questions, listening closely to primary care practices and evaluating our work, the tools and recommendations we make will evolve. Today, we’re sharing that we have decided to refresh what we categorize in the Core 4 – and we wanted to explain why.
Here are the new Core 4, and what led us to change them:
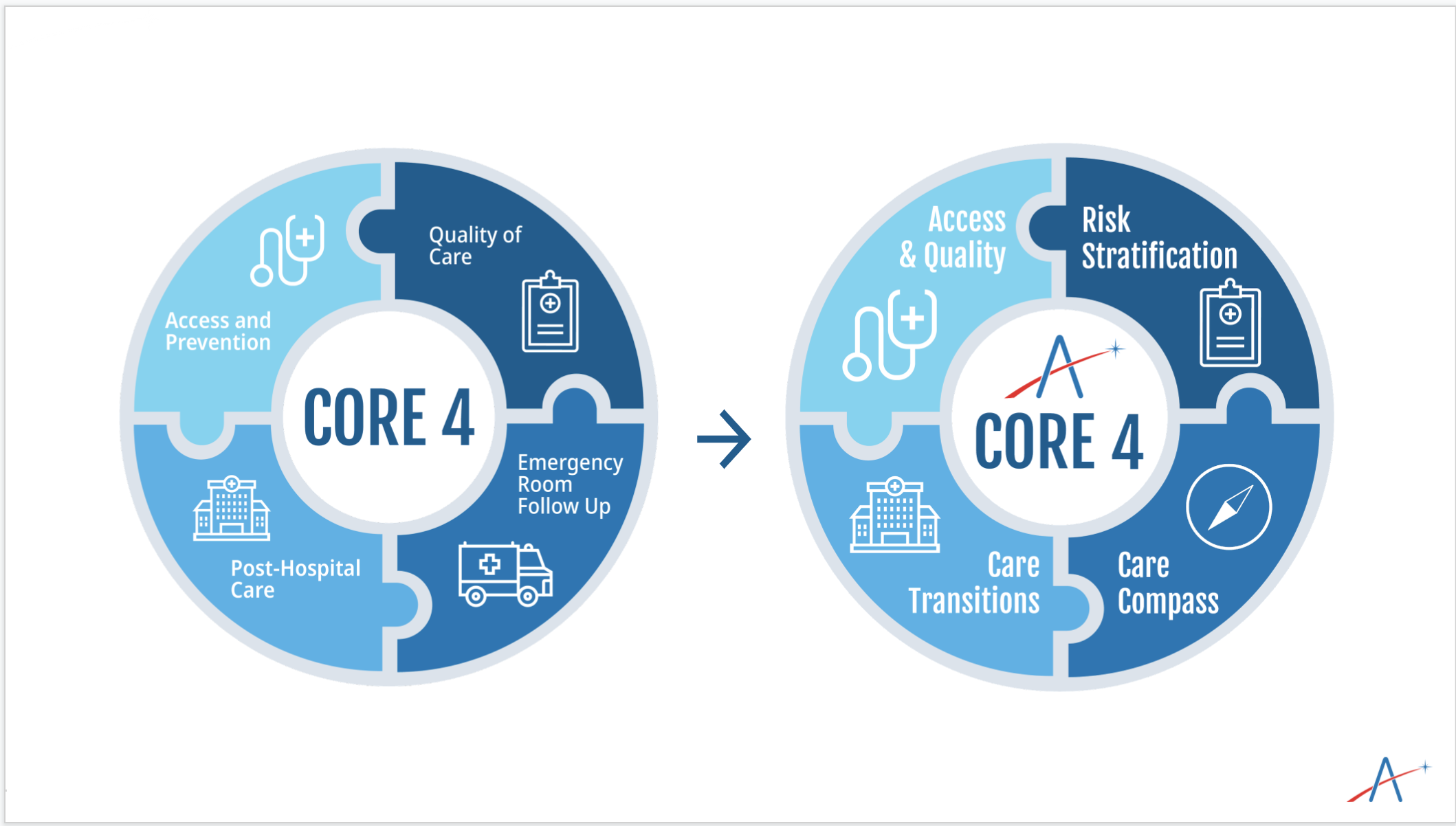
Care Transitions
Our original Core 4 included two categories – Emergency Room follow-up for patients who visit the ER, and Post-Hospital Care for patients who are returning home after a hospital stay. The evidence is clear that helping patients through these often confusing and stressful transitions between care settings leads to much greater patient satisfaction and much fewer adverse, avoidable and costly health care events.
After working closely with practices in our nationwide network, we recognized that ER follow up and Post-Hospital follow up are close companions. Both represent the opportunity to embrace vulnerable patients after an escalation in care. So we combined them into a single category called “Care Transitions” to emphasize the importance of continuity of care, regardless of where the patient received that care.
This new, combined category also gives us the opportunity to explore additional ways to manage care transitions in the future. We realize that patients travel within the medical neighborhood, and primary care should be empowered to do its job and wrap its arms around patients during those transitions.
Access and Quality
Previously, we labeled additional categories “Access and Prevention” and “Quality of Care,” which we visualized as distinct. In the original concept, “Access and Prevention” included our wellness and attribution efforts, and “Quality of Care” nodded to care gaps and appropriate diagnosis documentation.
But Quality isn’t just about satisfying performance metrics and documenting and communicating the acuity of the patient population we serve. At Aledade, our ambitions for true quality improvement extend beyond these high value activities. Our patients’ experiences during COVID-19 emphasized the importance of maintaining a true connection to primary care. Success in value based care necessitates “Access” and “Quality” as companions, encompassing wellness and prevention, attribution and quality improvement that will change the lives of patients and families.
Risk Stratification
Risk Stratification is a term of art in healthcare that refers to the alignment of patients with the right clinical initiatives, according to their clinical diagnoses and burden of illness. Aledade cannot satisfy our promise to leverage data to bring the best in customized care to our patients without understanding, completely and year after year, the diagnoses present for each patient.
Previously, we included the proper documentation of clinical diagnoses in the “Access and Prevention” category. But we have learned how vital it is to accurately document and communicate diagnoses during all visits and not just during wellness and prevention visits. At a broader level, this work allows practices to accurately reflect the acuity of the entire patient panel. The unique workflows necessary to achieve these goals encouraged “Risk Stratification” as a stand alone category.
Care Compass
All of this work to combine categories that were previously separate allowed us to open up a new, fourth category – the use of data to help patients get the best care complementary to the care they get in their PCP’s actual office. We’re calling it the “Care Compass.”
This “Care Compass” includes high value referral management work as well as the wraparound programs being pioneered by Aledade Care Solutions, the first of which is Comprehensive Advance Care Planning through Iris. Over time, this category will help us find new ways to empower independent primary care so they can provide even more care to their patients – care that helps improve outcomes and lower costs across the health care system.
A Note on Equity
One of the most important shifts in health care has been the explicit and clear focus on inequities in health, arising from the murder of George Floyd in 2020 and the demonstrations for equity that took place in communities all over the country. A fair question to ask is “Why is Health Equity not a category in the Aledade Core 4?”
Our answer is simple. Health equity cannot be confined to a single category. It must be a central consideration throughout each element of the Core 4.
We need to find new ways to expand access to neighborhoods and communities who have historically lacked that access. We need to help patients who leave the hospital and face new challenges in their care after an operation because of the condition of their home or neighborhood. We need to ensure that the highest risk patients, not just the patients who most frequently visit the doctor’s office, are fully diagnosed and documented so we can give them the care they need. And finally, we need to ensure every patient can get access to the wraparound services and care they need in close coordination with their primary care doctor.
The New Core 4
Access and Quality. Care Transitions. Risk Stratification. Care Compass.
The new Core 4 allows us to align the incentives in health care even better, so high quality patient care and the new way of doctors getting paid aren’t at odds with one another; in fact, they’re even more aligned so that better care leads to more resources for the quarterbacks of our health care system.
Ultimately, these four essential ingredients to value-based care are good for society as well. They help focus our efforts to bring better care to more high risk patients, and ensure that practices all across the country have a tried and true path to success in value-based care.
We’re excited to unveil these new Core 4 and begin to put them into practice across the more than a thousand practices who have joined an Aledade ACO – and the millions of patients those practices serve.
The Aledade “Core 4” is a registered trademark owned by Aledade, Inc.