Value-based care for primary care
Aledade is the nation's largest network of independent primary care. Our Accountable Care Organizations (ACOs) help practices and health centers improve patient outcomes and generate sustainable revenue.
What's value-based care?

Calculate potential revenue.
93%
of Aledade ACO partners earned shared savings in 2023 (compared to national average of 70%)*
Solutions designed for your unique needs
Achieve sustainability and clinical autonomy with Aledade’s data insights, support and business solutions.
Participating in the shared savings program with Aledade has helped our practice focus on caring for the whole patient, reducing fragmentation of care while also improving the quality of life of our clinicians. false
Aledade has helped us overall, not just with our Medicare patients. We see them as a partner in achieving our goals and achieving a high quality of care for our patients. That’s kind of the relationship we have with Aledade. false
true


Participating in the shared savings program with Aledade has helped our practice focus on caring for the whole patient, reducing fragmentation of care while also improving the quality of life of our clinicians.
Dr. Christine Meyer -
Internist & Founder Christine Meyer, MD & Associates | Exton, PA


Aledade has helped us overall, not just with our Medicare patients. We see them as a partner in achieving our goals and achieving a high quality of care for our patients. That’s kind of the relationship we have with Aledade.
Kristie Lenze
RN, CEO and CFO of Keystone Rural Health Consortia, located in rural Emporium, Pennsylvania
An ACO for you
No matter your practice size or setting, we have an ACO for you. Explore the map to see how Aledade is making a difference in your community.
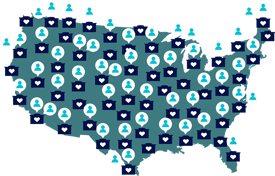
46
states + DC
20,000
clinicians
2.8M+
lives under management
*based on PY2023 MSSP results
