
By Britainy Barnes, Sr. Analyst, Policy
In October 2021, Broome et al. described using the Medicare Shared Savings Program (MSSP) as a “chassis” for innovation. This chassis could test new innovations with only a fraction of the effort required to build a new model from the ground up and establish the MSSP infrastructure as the starting point for many providers, not a competitor to new Innovation Center models. To further demonstrate this idea, the Aledade policy team developed a series of blogs describing how this would work for four innovations: primary care capitation, value-based insurance design, addressing inequity in health care, and incorporating desired elements from the Next Generation ACO model.
Everyone agrees that primary care payment reform is essential for care redesign. The idea of offering capitation payments to primary care providers is not novel for CMMI— from Track 2 in CPC+ or the All-Inclusive Population-Based Payment (AIPBP) in Next Gen ACOs, to the newer Primary Care First and Primary Care Capitation in ACO REACH (formerly Direct Contracting). While it is too early to evaluate PCF and DC, the most recent CPC+ evaluation report showed that CPC+ practices participating in MSSP outperformed those not in MSSP.
We already know that MSSP has saved money, especially in physician-led ACOs. What if we offered primary care capitation in an environment that has been proven to save money while also providing a means to distance MSSP from its reliance on fee-for-service?
In this brief, we are proposing a new, simple, primary care capitation model housed within MSSP. It would create the opportunity for ACOs to receive quarterly payments for their attributed patients, which would allow MSSP participants to continue driving innovation in care delivery rather than having their revenue be dependent on volume. ACOs would have the freedom to deliver care wherever and by whoever is best suited. Additionally, Medicare’s prior experience with such models makes our proposal simple to implement, without disrupting the total cost of care calculations established in MSSP.
Incorporating a Capitation Model Into MSSP
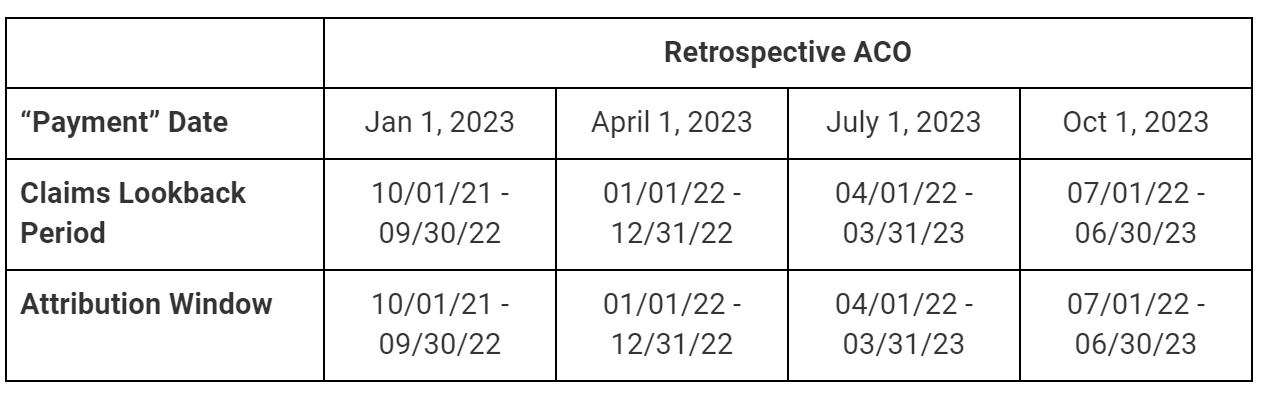
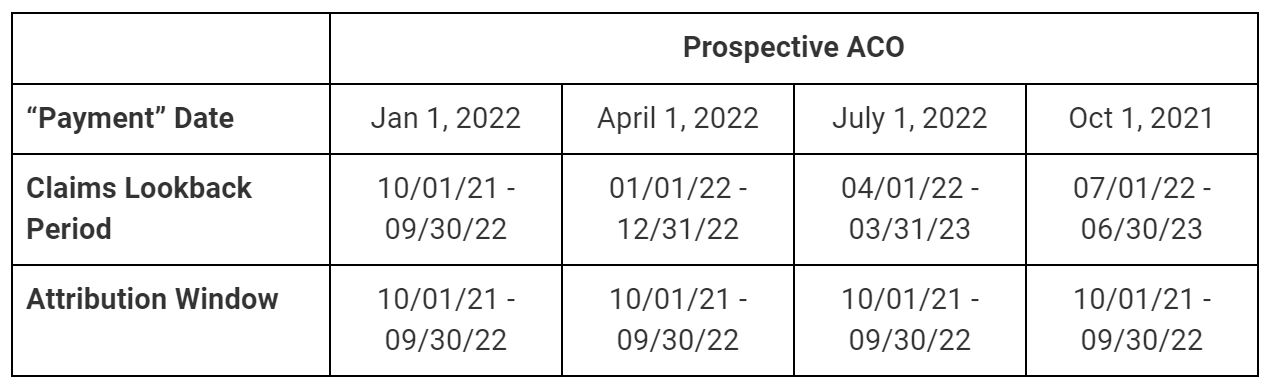
To calculate the Primary Care Capitation (PCC) Amount, CMS should use the most recent list of beneficiaries that are attributed to the ACO.1 For ACOs with retrospective attribution, the lookback period for claims would be the same as the assignment window. For ACOs with prospective attribution, the lookback period would be updated quarterly as shown in the tables below. The historical claims2 from this same period that were for covered services and provided by ACO participants would then be adjusted for any changes to the Medicare physician fee schedule to create the Historic PCC. By pairing this model with total cost of care responsibility, we avoid having to nitpick which services are included or excluded from the capitation calculation and are able to offer a simplified list of services to consider.
ACOs would also receive 40 percent of their Historic PCC as a bonus to help drive innovation. This bonus would be treated as a non-claims based payment (NCBP) for benchmarking and total cost of care purposes.
There are three reasons for doing historical payments plus a 40 percent bonus. First, it is similar to the Enhanced PCC amount received by DCEs. For a DCE that has a primary care historical spend of 5 percent, a 2 percent Enhanced PCC represents a 40 percent increase in primary care revenue. Second, by treating the bonus as a NCBP it prevents CMS from having to make adjustments for patients that lose attribution from one quarter to the next. Third, it incentivizes primary care providers to do more under their own umbrella, in lower-cost settings of care, since the care they provide in one year will be used to calculate the historical PCC for the following year.
Additionally, we believe the model should only offer a full capitation as partial primary care capitation creates misaligned incentives. For example, the flat-service-fee of PCF removes the incentive to provide “good FFS” such as TCMs and AWVs while retaining the negative FFS feature of volume equaling revenue.
Operationalizing a primary care cap in MSSP would be done similarly to the All-Inclusive Population Based Payment (AIPBP) of NextGen and the capitation mechanisms in ACO REACH. Providers in MSSP would have a waiver or track available to them that allows them to have their primary care claims for attributed patients reduced by 100% and receive monthly payments for the services covered by the cap in place of FFS payments. Much like the ACO REACH capitation mechanisms, providers would continue to submit all claims to CMS. CMS would then adjudicate the claim and determine the payment amount to providers based on whether the patient appeared on the most recent attribution list. More details on claims processing in DC can be found in Section 4 of the Direct Contracting Model PY 2022 Financial Operating Policies and Transmittal 10820 from the Demonstration Manual.
Example
For the Q1 2023 (January 1, 2023) payment, the claims lookback period would be October 1, 2021 through September 30, 2022 for all ACOs. During this time period, the 10,000 beneficiaries that are attributed to the ACO had total eligible claims of $4.8 million. After adjusting these claims to match 2023 physician fee schedule changes to RVUs and updates to the conversion factor, the new total is $5 million. A 40% bonus is applied, bringing the final lump sum the ACO would receive for the quarter to $1.75 million ($5M × 140%/4) or $58.33 PMPM ($1,750,000 ÷ 3 months/10,000 beneficiaries).
For ACOs with prospective attribution, the calculation would be the same, but some dates differ slightly. While the claims lookback period would update each quarter, the attribution window would remain October-September. As such, it is expected that the PMPM and quarterly lump sum payment to ACOs with prospective attribution would fluctuate less than the payment to ACOs with retrospective attribution whose patient lists would change quarterly.
While a 40 percent increase in payments to PCPs might sound extreme, the dollar amount is not all that different from what was paid to Track 2 CPC+ practices. The average care management fee was $336 per patient per year. Sticking with the above example of a $1.75M quarterly payment, this would represent an additional $200 per patient over historic costs. Primary care capitation is a cheaper solution than CPC+ and, more importantly, providers are accountable for this increased cost of care which is reflected in the settlement at the end of the year. As such, these payments should be considered costs of care for purposes of reconciliation and should not be reconciled against actual services billed.
Ensuring Equity is at the Forefront of Model Development
As CMS and CMMI examine models through an equity lens, something to keep in mind is that FFS reimburses providers in health professional shortage areas an additional 10%. When calculating the historical payments, these HPSA bonuses should be factored into the calculation.
Finally, the strength of this primary care capitation model is that it empowers practices to do what’s best for them and their patients. For a practice with a stable, established, and large Medicare panel, capitation might be what they’ve been yearning for. However, an FQHC with a small Medicare population might be better off continuing to receive the PPS. Regardless of their decision on the capitation model, neither of these practices have to miss out on participating in a total cost of care model when primary care capitation is an option within MSSP. The same is not true for ACO REACH. The FQHC is barred if capitation is not right for them.
Once more race, ethnicity, and socioeconomic data are reliably available, future iterations of the MSSP primary care capitation model can include an adjustment to the bonus payment that accounts for these factors.
It has been shown that providing wraparound services to address patients’ socioeconomic barriers has a negative association with hospitalizations and emergency department utilization. ACOs and primary care providers are ideally positioned to partner with local entities to help patients access these services. There is no CPT code for doing this, but a primary care capitation bonus could go a long way in making their provision economically feasible.
Next Steps
In its recent white paper, CMS states that “advanced primary care and accountable care models are central to driving growth in the number of beneficiaries in accountable care relationships.” By pairing a primary care capitation model directly with an established, successful accountable care model, CMS can achieve its strategic objectives of driving accountable care, supporting care innovations, and achieving system transformation while ensuring equity is at the forefront. When coupled with the other models in our series, a chassis for CMS to achieve its 10 year vision and meet all five objectives outlined in its white paper is created.
Including this model as an option within MSSP by January 1, 2023 can fuel growth in the program by attracting providers who have their eye on ACO REACH but are wary of resetting their benchmark and adjusting to new risk adjustment methodologies. Additionally, it can aid in program retention by providing the next step for participants looking to move away from fee-for-service. The level of effort required to stand-up this model is minimal since the claims-processing system requirements already exist from prior models and the math is relatively straightforward. ACOs that decide to participate in primary care capitation alongside MSSP will do so because they believe a new payment model would help them improve care without the need to evaluate whether it is a model that provides a more favorable benchmark.
1 Attributed patient lists for ACOs under retrospective assignment would follow a similar timeline to the one used in Primary Care First (PCF) but be limited to a 12 month lookback period. For ACOs under prospective assignment, attributed patients are those that appear in the list provided to ACOs near the start of the performance year.
2 Primary care services covered in the cap should be the same codes as those used to determine attribution for the current performance year.
