
By Casey Korba, Director of Policy
Most headlines related to the 2024 Proposed Physician Fee Schedule are similar to recent years, focusing on cuts to fee-for-service (FFS) payments. But this year’s rule also introduces several positive policy changes for the Medicare Shared Savings Program (MSSP) – great news for primary care physicians who plan to participate in an Accountable Care Organization (ACO) next year. It is clear from this year’s proposals that CMS is focused on helping physicians carry out its 2030 accountable care goal. Let’s take a look at how these provisions would pave the way.
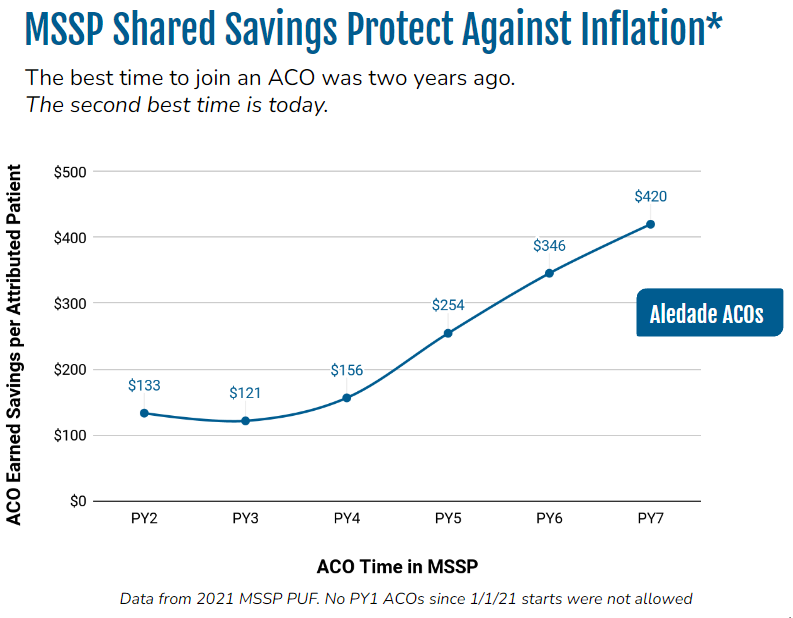
Fee-for-service is eroding over time, while earned ACO savings positively compound.
The conversion factor (the number of dollars assigned to an RVU) is slated to drop 3.37 percent from 2023 to 2024. This number has been on a downward slope, but every year since the pandemic, Congress has intervened with a temporary fix by year’s end to lessen the impact. We predict that will happen again this year. Next year, there could be enough momentum for a more permanent fix, with discussion of indexing physician pay off the Medicare Economic Index, a measure of inflation faced by physicians with respect to their practice costs and general wage levels.
Over the last decade, CMS has added more care management codes to address the needs of complex patients. In this proposed rule, CMS is proposing G2211 (add-on code for E&M visits associated with medical care services that serve as the continuing focal point for all needed health care services and are inherently associated with primary care) and GXXX5 (Social Determinants of Health Risk Assessment), which would provide an additional $16 and $18 respectively when billed (if finalized as proposed).
For the past several years, Congress has been putting annual Band-Aids on FFS while ACO savings compound each year without the brinkmanship that comes with Capitol Hill. For clinicians in the MSSP, the financial power of being in an ACO means that earned savings revenue can increase over time. While inflation eats away at FFS, the reverse is happening in MSSP.
Aledade and the ACO community’s persistence has paid off in the proposed rule in many areas including attribution, quality reporting, benchmarking, risk adjustment, and the future of MSSP.
Attribution
By law, beneficiaries have to see a physician to be eligible for attribution. Nurse practitioners and physician assistants only count toward assignment to an ACO if there is a qualifying physician visit.
CMS is proposing to extend the period for that qualifying visit to happen from 1 year to 2 years. This will make it easier to attribute beneficiaries who may not have complex health needs or need to see a physician every year. By increasing this window by 12 months, CMS estimates that nearly 3 percent, or around 1 million beneficiaries, would become eligible for MSSP if the proposal is finalized. This will help CMS reach their goal of having 100% of Medicare beneficiaries in an accountable care arrangement by 2030.
Quality reporting
CMS has set a goal to transition to electronic clinical quality measures (eCQMs) using all-patient, all-payer reporting. Aledade and the ACO community have focused the last few years on communicating and providing data on the time and costs associated to implement these requirements, including having to aggregate data across all practices using different electronic health records.
The move to eCQM means that ACOs have to report on all patients–not just Medicare beneficiaries or those who have a primary care relationship with the ACO’s clinicians. Unintended consequences include having to have specialists provide services that are usually provided in primary care. (Most patients do not expect a depression screen if they are seeing a dermatologist for a rash, for example.) In some circumstances, meeting the quality measure could require more tests than Medicare will even pay for. It could also lead to lower scores for ACOs that serve a large proportion of traditionally underserved patients because there is no way to account for differences in Medicaid or the uninsured.
The proposed rule’s new quality option for ACOs in MSSP shows that CMS has been listening. The Medicare Clinical Quality Measures (CQM) would require ACOs to report only on Medicare beneficiaries, rather than the all-patient, all-payer reporting CMS had proposed previously. It would also limit the requirement to Medicare beneficiaries who receive a primary care service from the ACO.
In performance year 2024, ACOs would have the option to report quality data utilizing three different methods: CMS Web Interface measures, eCQMs, and/or MIPS CQMs collection types. In performance year 2025 and subsequent performance years as determined by CMS, ACOs would have the option to report quality data utilizing the eCQMs, MIPS CQMs, and/or Medicare CQMs collection types.
Risk adjustment
Risk adjustment has its flaws, but is absolutely necessary to properly measure practices that serve more complex and vulnerable patients. CMS is proposing a modified use of the CMS-HCC risk adjustment model to account for the new model version (v28) laid out in the Medicare Advantage Rate Notice for 2024. If the proposal is finalized, the same model version will be used in benchmark and performance years.
This is another area where Aledade and other stakeholders have presented data to CMS on the importance of symmetry so that the risk ratio reflects population health changes rather than model changes. CMS listened, did their own analysis, and came to the conclusion that this symmetry is important to prevent any unintended distortions in benchmark and risk calculations. One note is that this is only for new ACO contracts in 2024 under the proposal. We believe it should be for all ACOs.
Benchmarking
Aledade has made the case to CMS that allowing negative adjustments in the benchmarking process serves to deter participation and makes it harder for higher cost health care organizations to succeed. CMS revisited the policy and is proposing to eliminate negative regional adjustments. This is great news for ACOs that have populations with greater health needs as well as large health systems that have had historically higher costs driven by high utilization but are looking to the future of value.
The future of MSSP
CMS is interested in thinking through future policies that strengthen MSSP and is soliciting comments in different areas, including what it could look like to incorporate a track with higher risk and potential reward, continuing to evolve the benchmark, and policies to promote ACO collaboration with community-based organizations (CBOs).
Aledade has long advocated for MSSP innovations such as having primary care capitation and waiving co-pays for primary care, and we have begun to examine promising strategies for collaboration between ACOs and CBOs to address the social drivers of health. We look forward to sharing more of our ideas in our comments to CMS.
The 2024 Proposed PFS represents years of CMS listening to the ACO community and taking a data-driven approach to reducing barriers to participation in accountable care and advancing primary care. Policy rarely moves fast, but it does move, and Aledade looks forward to continuing the dialogue and working with the ACO community and CMS to improve care delivery and health outcomes across the country.
CMS’s hands are tied on the overall payment reduction in FFS and we eagerly await movement on Capitol Hill. For everything else we simply say “well done.” CMS continues to support investment in primary care and overall care management by putting in the time to make data-driven decisions. This work is definitely wonky but also critical to ensuring the long-term success of the accountable care movement.
The CMS deadline to join an ACO for the 2024 performance year is August 1, 2023. Secure your spot in an Aledade ACO today.
* Based on past performance. Shared savings not guaranteed.
